Pelvic pain and heavy bleeding during periods are incredibly common—so common that one in five women are told these symptoms are “normal.” But they are often signs of overlooked conditions like endometriosis and adenomyosis, two diseases that are often confused.
In this blog, we’ll break down the differences between them so you can understand what each condition means, how symptoms show up, and why these distinctions matter for your health.
Understanding the Difference Between Endometriosis and Adenomyosis
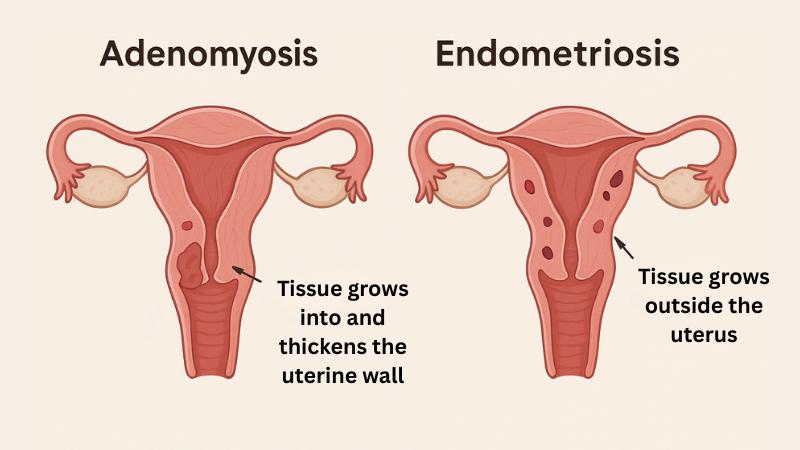
Although both these conditions involve endometrial-like tissue, location is the key difference between endometriosis and adenomyosis.
Endometriosis is characterized by tissue similar to the uterine lining that grows outside the uterus, often on the ovaries, fallopian tubes, or pelvic lining.
Meanwhile, adenomyosis is a condition in which the uterine lining grows into and thickens the muscular uterine wall.
Adenomyosis and Endometriosis vs. Other Uterine Conditions
Endometriosis and adenomyosis can share symptoms with other conditions, like uterine fibroids, which are noncancerous growths in the uterus. These growths can cause heavy bleeding, pelvic pain, and pressure. Since symptoms of these uterine conditions overlap, getting a proper evaluation from a specialist can help determine the cause.
Adenomyosis Symptoms Versus Endometriosis Symptoms
Both endometriosis and adenomyosis have four stages, including early, moderate, severe, and advanced stages. The early stages tend to have milder or even no symptoms, while advanced stages have more intense symptoms, such as severely painful periods.
It’s also possible to have adenomyosis and endometriosis at the same time, which may make symptoms more intense.
While symptoms of endometriosis and adenomyosis may overlap, distinct characteristics can help differentiate the two, including:
Common Symptoms of Endometriosis
Some of the uterine endometriosis symptoms you may come across:
- Severe pelvic pain, especially during periods
- Pain during sex, bowel movements, or urination
- Spotting between periods
- Infertility
Common Symptoms of Adenomyosis
Some of the uterine adenomyosis symptoms you may come across:
- Heavy or prolonged menstrual bleeding
- Painful menstrual cramps that worsen over time
- A feeling of pelvic pressure or fullness
Since symptoms of endometriosis and adenomyosis are so similar, the only way to determine the specifics of your condition is by visiting a specialist for a diagnosis.
How Do Adenomyosis and Endometriosis Develop?
Understanding how adenomyosis and endometriosis develop helps explain their symptoms and guides treatment options. Although the exact causes of these conditions are still being researched, several theories and potential risk factors have been identified by medical professionals.
Why Endometriosis Develops
Some of the potential causes of endometriosis include:
- Retrograde menstruation: When menstrual blood flows backward, going into the pelvic cavity instead of out through the vagina.
- Immune dysfunction: The immune system fails to clear misplaced endometrial cells.
- Cellular metaplasia: A process where several cells transform into endometrial-like tissue.
- Genetics: Having a family history of endometriosis can increase the risk of developing it.
Why Adenomyosis Develops
For adenomyosis, potential causes can include:
- Childbirth or uterine surgery: Physical changes or injury to the uterine lining may allow endometrial tissue to grow into the uterine wall.
- Fetal development: Misplacement of endometrial tissue before birth may lead to adenomyosis later in life.
- Hormonal influences: High estrogen levels may stimulate the growth of endometrial tissue within the uterine wall.
- Uterine inflammation: Chronic inflammation may disrupt the boundary between the endometrium and myometrium, enabling tissue growth into the muscle layer.
- Invasive tissue growth: Endometrial tissue may penetrate the uterine muscle due to a breakdown in the barrier between the layers of the uterus.
- Genetics: Having a family history of adenomyosis may increase the risk of developing it.
Can You Have Both Endometriosis and Adenomyosis?
It is possible to be diagnosed with both endometriosis and adenomyosis. However, if only one condition is treated or screened for, the other may go unnoticed, prolonging symptom relief. A comprehensive evaluation by an expert interventional radiologist can help identify both conditions and develop a treatment plan that addresses all underlying sources of pain and bleeding.
Schedule a Diagnosis With a Specialist
Diagnosing Endometriosis vs. Adenomyosis
There are diagnostic processes and techniques available to provide a better idea of whether endometriosis or adenomyosis might be causing unwanted symptoms.
How Endometriosis Is Diagnosed
Endometriosis is often diagnosed through a laparoscopy, a minimally invasive procedure that allows doctors to view the uterus directly and, if necessary, remove abnormal tissue.
Imaging techniques such as ultrasound or MRI may detect large or deeply embedded lesions, but they may miss smaller growths. Diagnosis is more common in younger women experiencing chronic pelvic pain or difficulty conceiving.
How Adenomyosis Is Diagnosed
Adenomyosis is often detected through imaging tests such as MRI or ultrasound, which reveal changes in the uterine wall. A pelvic exam may reveal an enlarged or tender uterus, leading to further examination using these imaging tests.
This condition is more common in women over the age of 30, particularly those who have given birth, but it can still occur in individuals of various ages and reproductive histories.
Treatment Options for Endometriosis and Adenomyosis
Since endometriosis and adenomyosis differ in how they develop and where they occur, treatment approaches can vary widely.
Endometriosis Treatment Options
Endometriosis has three main treatment options:
- Hormonal birth control or GnRH agonists to suppress growth.
- Pain management with NSAIDs.
- Laparoscopic surgery to remove lesions and scar tissue.
A healthcare provider can help develop a tailored treatment plan based on the severity of endometriosis symptoms and individual needs.
Adenomyosis Treatment Options
The treatment of adenomyosis may include:
- Hormonal therapy to reduce bleeding and pain.
- Hysterectomy in severe, treatment-resistant cases.
- Non-surgical procedures, like uterine artery embolization (UAE).
An interventional radiologist can help you determine the best treatment plan based on your symptoms.
Uterine Artery Embolization (UAE): A Minimally Invasive Option for Adenomyosis
Uterine artery embolization (UAE) is an FDA-approved outpatient procedure that blocks blood flow to abnormal uterine tissue, shrinking it and relieving symptoms.
The benefits of uterine artery embolization include:
- Preserving the uterus
- No general anesthesia
- No surgical scarring
- Short recovery time
- High satisfaction rate
For those looking to avoid invasive surgeries with lengthy recovery times, UAE can be a viable minimally invasive alternative.
Getting the Right Diagnosis and Support
Understanding the difference between endometriosis and adenomyosis is the first step toward relief. USA Fibroid Centers provides diagnoses and minimally invasive solutions, like UAE, to treat adenomyosis and alleviate symptoms.
For individuals experiencing symptoms that may be related to endometriosis or adenomyosis, schedule a consultation today to take the first step towards answers and managing your symptoms.
FAQs About Endometriosis and Adenomyosis
Is adenomyosis the same as endometriosis?
Adenomyosis and endometriosis are not the same and are two separate uterine conditions, although they have similar symptoms. Adenomyosis grows into the uterus’s muscular wall, while endometriosis develops outside the uterus, usually on pelvic organs.
Can adenomyosis lead to endometriosis?
Adenomyosis does not lead to endometriosis, but individuals can have both conditions at the same time, as they develop in different locations in the uterus.
Can endometriosis or adenomyosis return after treatment?
Since endometriosis and adenomyosis are chronic conditions, recurrence is possible depending on factors like the severity of the condition and the type of treatment received. This is why it’s so important to have a long-term care plan with your doctor that includes regular check-ins and follow-up care to manage your symptoms effectively.