Navigating your 40s often involves significant physical changes. When heavy cycles and mood fluctuations occur, it can be difficult to distinguish between hormonal shifts and anatomical issues. Navigating the overlap between perimenopause and uterine fibroids is complex, as both conditions can cause unpredictable, heavy bleeding and pelvic discomfort.
While perimenopausal shifts mark a natural transition toward menopause, uterine fibroids are non-cancerous growths that often thrive on the hormonal fluctuations occurring during this stage. Recognizing early signs is the first step in obtaining an accurate diagnosis and maintaining your quality of life.
Understanding What Perimenopause Is
Perimenopause is the natural transition toward the end of your reproductive years, occurring as the ovaries gradually decrease hormone production. Being perimenopausal means your estrogen and progesterone levels may fluctuate unpredictably, causing your menstrual cycle to become erratic or irregular.
The most prominent feature of being perimenopausal is declining estrogen, which eventually leads to the cessation of ovulation. Although cycles are often unpredictable, pregnancy remains possible until you reach official menopause—defined as 12 consecutive months without a period. Once this milestone is reached, estrogen levels remain consistently low, and the ability to conceive naturally ends.
When Does Perimenopause Start?
The transition into perimenopause typically begins in the mid-40s, often serving as a multi-year lead-up to menopause. The average age of perimenopause is approximately 45, though the timeline varies significantly by individual.
When asking, “When does perimenopause start?” it is important to note that while the typical age for perimenopause is the 40s, some women notice early perimenopause symptoms in their late 30s. If cycles become irregular before age 40, it may be categorized as premature menopause or primary ovarian insufficiency.
How Long Does Perimenopause Last?
The duration of perimenopause typically varies anywhere from four to eight years. It officially ends when a woman has gone 12 consecutive months without a period, marking the beginning of menopause.
What Are Common Symptoms During Perimenopause?
Perimenopause isn’t a single event; it can last anywhere from two to ten years. As estrogen levels spike and dip unpredictably, your body sends out several “red flags.”
The most common signs include:
- Irregular Cycles: Periods that are suddenly much shorter, longer, or skip months entirely.
- Vasomotor Symptoms: The classic “hot flashes” and night sweats are caused by the hypothalamus reacting to estrogen withdrawal.
- Sleep Disruptions & Mood Swings: Often linked to declining progesterone, leading to anxiety or “brain fog.”
- Heavy Periods: While many expect periods to lighten, estrogen spikes can actually cause heavier bleeding and worse cramping.
Why Fibroids Often Go Undetected During Perimenopause
Uterine fibroids are noncancerous growths of muscle and tissue that develop in or on the wall of the uterus. While they aren’t associated with an increased risk of uterine cancer, they can range in size from seeds, unnoticed by the human eye, to bulky masses that can enlarge the uterus.
The primary reason they can remain undetected is that fibroid symptoms frequently overlap with the natural chaos of perimenopause symptoms. When a person experiences heavy bleeding or irregular cycles, they often attribute it to the change rather than an underlying structural issue like a fibroid.
Why Fibroid Symptoms Vary
Not every fibroid makes its presence known. Whether a fibroid is asymptomatic or a source of significant discomfort depends on three main factors:
- Location: Submucosal fibroids (growing into the uterine cavity) can cause heavy bleeding even if they are small. Subserosal fibroids (on the outer surface) may grow quite large before pressing against the bladder or bowel.
- Size: Smaller fibroids may go unnoticed, while those the size of a grapefruit can cause a visible “fibroid belly.”
- Number: Multiple fibroid clusters can increase uterine size, causing a persistent feeling of pelvic fullness often mistaken for weight gain.
At What Age Do Fibroids Commonly Occur?
Uterine fibroids are most commonly diagnosed in women between the ages of 30 and 50. While they can develop at any time during the reproductive years (after puberty and before menopause), they are most prevalent during the 40s and early 50s, when estrogen levels are often at their peak or fluctuating significantly during perimenopause.
After menopause, when estrogen levels drop, fibroids typically stop growing and may even shrink, making new occurrences much less common in older age.
Do Fibroids Grow or Shrink During Perimenopause?
Fibroids can often surge in growth during perimenopause. While estrogen eventually declines, the sharp hormonal spikes leading up to menopause act as “fuel,” reawakening dormant fibroids and triggering sudden pain or heavy bleeding.
Fibroids or Perimenopause? Understanding the Overlap
Distinguishing between these conditions is difficult because both involve irregular bleeding perimenopause patterns. Fibroids and perimenopause frequently occur together, making professional diagnosis essential.
Perimenopause vs. Uterine Fibroids: Symptom Comparison
| Symptom | Perimenopause (Hormonal) | Uterine Fibroids (Anatomical) |
| Bleeding Pattern | Irregular timing; periods may skip or occur closer together. | Consistently heavy or prolonged periods; may include large clots. |
| Physical Sensation | General bloating or tenderness. | Distinct pelvic pressure, “fullness,” or a visible abdominal bulge. |
| Pain Location | Systemic (joint aches, headaches). | Localized (lower back, leg aches, or pelvic cramping). |
| Organ Interference | Minimal impact on bladder/bowel. | Frequent urination or constipation due to physical pressure. |
| Systemic Signs | Hot flashes, night sweats, and mood shifts. | Anemia-related fatigue due to chronic blood loss. |
Many women in their 40s experience fibroids during perimenopause simultaneously. Because fibroids are estrogen-dependent, the hormonal surges of this transition can cause existing growths to enlarge. If you experience “flooding” (soaking a pad or tampon every hour) or pelvic pain, seek a specialized pelvic ultrasound or vascular consultation.
Perimenopause vs. Uterine Fibroids: Symptom Overlap
While perimenopause is a hormonal transition, and fibroids are physical growths, their symptoms often overlap in frustrating ways, such as:
- Changes in Menstrual Flow
The most common overlap is fibroids and perimenopause bleeding patterns that suddenly feel unpredictable. Perimenopause often causes heavy periods due to fluctuating estrogen. Similarly, fibroids can increase the surface area of the uterine lining or prevent the uterus from contracting properly, leading to soaking through pads or tampons at an alarming rate.
- Spotting Between Periods
If you’re noticing spotting or bleeding between periods, fibroids are often the culprit, particularly submucosal fibroids that bulge into the uterine cavity. While perimenopause can cause irregular cycles where you spot because ovulation is hit-or-miss, consistent mid-cycle bleeding is a sign that a physical growth might be irritating the lining.
- Pelvic Pressure and Bloating
That full feeling in your lower abdomen, often called the fibroid pooch, can easily be mistaken for perimenopausal weight gain or digestive bloating. However, if the pressure feels constant or is accompanied by a frequent urge to urinate, it’s more likely the physical bulk of a fibroid pressing on surrounding organs.
- Fatigue and Brain Fog
You might blame perimenopause for your low energy, but if you have fibroids and experience heavy bleeding, you could actually be dealing with anemia. A significant loss of iron from heavy cycles leads to exhaustion and “fog” that no amount of sleep can fix.
A proper diagnosis is required to be able to choose the right treatment. Treating hormonal shifts won’t shrink a physical tumor, and ignoring fibroids can lead to unnecessary pain. An ultrasound or MRI is the best way to distinguish between these conditions.
Bleeding Changes to Pay Attention To
It is a myth that every cycle change is “just part of the process.” Heavy bleeding in perimenopause should always be evaluated.
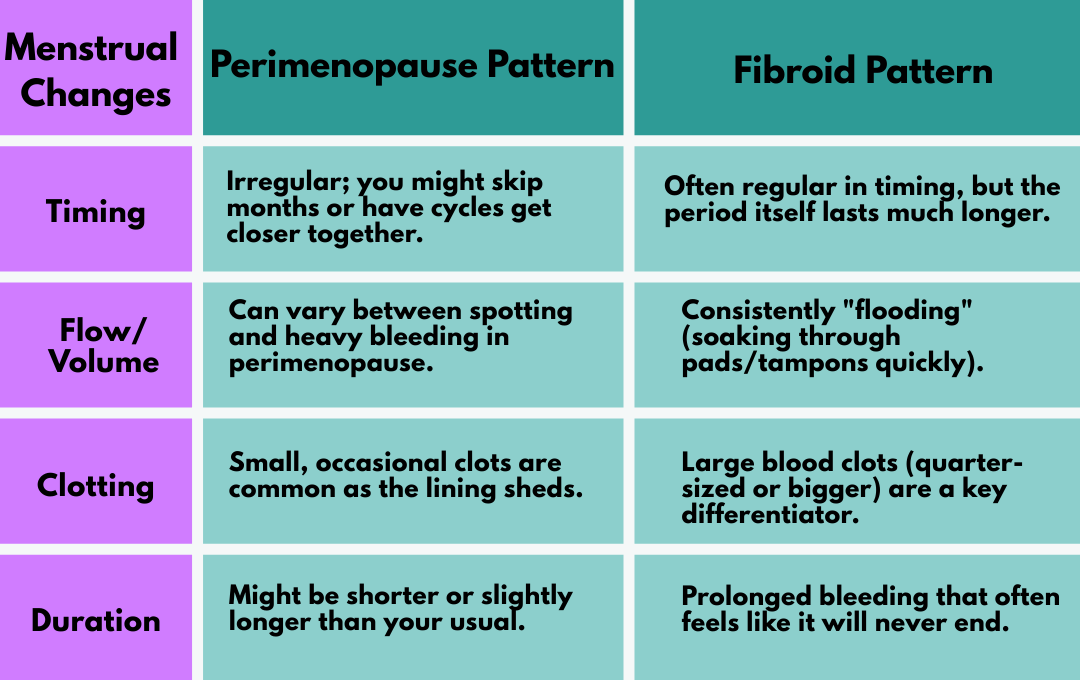
Fibroids and Perimenopause Bleeding Patterns
It is important to evaluate any change in your cycle. While perimenopause can cause the occasional heavy or skipped period, the nature of the bleeding is often different.
- Perimenopause Bleeding: Usually characterized by cycles that are shorter, longer, or lighter/heavier due to missing ovulations. You might skip two months and then have a normal period.
- Fibroid Bleeding: Typically involves soaking through a pad or tampon in an hour and often includes large blood clots. This bleeding is often prolonged, lasting more than 7 days.
Distinguishing between “irregular cycles” and “symptomatic heavy bleeding” can be the difference between a natural transition and a medical condition requiring a pelvic ultrasound.
When Does “The Change” Become a Crisis?
It is essential to distinguish between the gradual, manageable shifts of hormonal aging and symptoms that signal a medical event. While perimenopause symptoms like hot flashes are expected, they should never be debilitating.
At USA Fibroid Centers, our specialists often see women who have been told to “just wait it out,” only to discover that their transition is being complicated by uterine fibroids. You should seek a professional evaluation if you experience:
- “Flooding” During a Period: Soaking through a pad or tampon in a single hour is an acute symptom, not a standard part of perimenopause. This level of blood loss often signals that fibroids are reacting to estrogen spikes, leading to severe anemia.
- Extended Bleeding: Periods that last more than seven days or occur with large, painful clots.
- Physical Pressure: Sharp pelvic pain or a frequent, urgent need to urinate caused by fibroids pressing against the bladder.
Beyond heavy bleeding, you should consult a physician for sharp pelvic pain, bleeding that lasts more than seven days, or a frequent, urgent need to urinate. These signs of perimenopause may actually be symptoms of fibroids. If your symptoms feel urgent rather than a slow, manageable change, prioritize a diagnostic ultrasound and consult a fibroid specialist to ensure you are receiving the right care.
Get Answers & Expert Care With USA Fibroid Centers
It is important to distinguish between the gradual shifts of hormonal aging and symptoms that require medical attention, like fibroids and perimenopause. While signs of perimenopause, like irregular cycles or hot flashes, are expected, they should not be debilitating.
If your symptoms feel urgent rather than a slow, natural change, a pelvic ultrasound is the first step toward clarity. Our interventional radiologists specialize in identifying fibroids and offer Uterine Fibroid Embolization (UFE)—a minimally invasive, non-surgical treatment.
By choosing UFE, you can effectively shrink fibroids and stop heavy bleeding while preserving your uterus and natural hormone levels. Don’t let fibroids dictate your transition into menopause.
FAQs About Perimenopause & Fibroids
Can fibroids get worse during perimenopause?
Fibroids can get worse during perimenopause due to the high levels of estrogen that can occur during hormonal fluctuations in your 40s, with symptoms like heavy bleeding intensifying.
What are the 4 stages of perimenopause?
The 4 stages of perimenopause are:
- Very Early (subtle cycle changes)
- Early Transition (cycles vary by 7+ days)
- Late Transition (skipping 60+ days)
- Menopause (12 months without a period)
How can you check if you’re in perimenopause?
Determining if you’ve entered perimenopause is rarely as simple as a single blood test. Because hormone levels fluctuate wildly during this transition, standard FSH (Follicle-Stimulating Hormone) tests often provide an incomplete picture. Instead, the most accurate “check” is a comprehensive review of your symptom patterns and menstrual history.
Can You Still Get Pregnant During Perimenopause?
You can still get pregnant during perimenopause as long as you are still having a period and ovulation is occurring. If you do not wish to become pregnant, contraception is still necessary during perimenopause until you have officially reached menopause.