For many women, menstrual cramps are an unpleasant but familiar monthly occurrence. In the early years, they might be uncomfortable yet manageable with a hot water bottle or an over-the-counter painkiller. But what happens when those cramps begin to feel sharper, last longer, or disrupt your daily life more as the years go by? If you’ve noticed your period pain getting worse with age, you’re not alone and you’re not imagining it. While hormonal changes over time can make periods feel different, in some cases, worsening menstrual pain can be a sign of an underlying condition that deserves attention. Understanding what’s normal, what’s not, and when to seek help is essential for protecting your reproductive health.
Understanding Menstrual Pain (Dysmenorrhea)
Menstrual pain, or dysmenorrhea, comes in two forms. Primary dysmenorrhea is caused by natural contractions of the uterus as it sheds its lining, while secondary dysmenorrhea is linked to underlying conditions such as fibroids or endometriosis. Early in life, many women experience primary dysmenorrhea, which can vary in intensity but generally follows a predictable pattern. However, as the body ages, hormonal shifts, lifestyle changes, and medical conditions can all influence how and how much you feel period pain.
Why Period Cramps Might Worsen with Age
One of the most common reasons is hormonal fluctuation, especially during your 30s and 40s when perimenopause begins to set in. The natural ups and downs of estrogen and progesterone can increase the production of prostaglandins — hormone-like substances that make the uterus contract more strongly. Stronger contractions often mean more intense cramps.
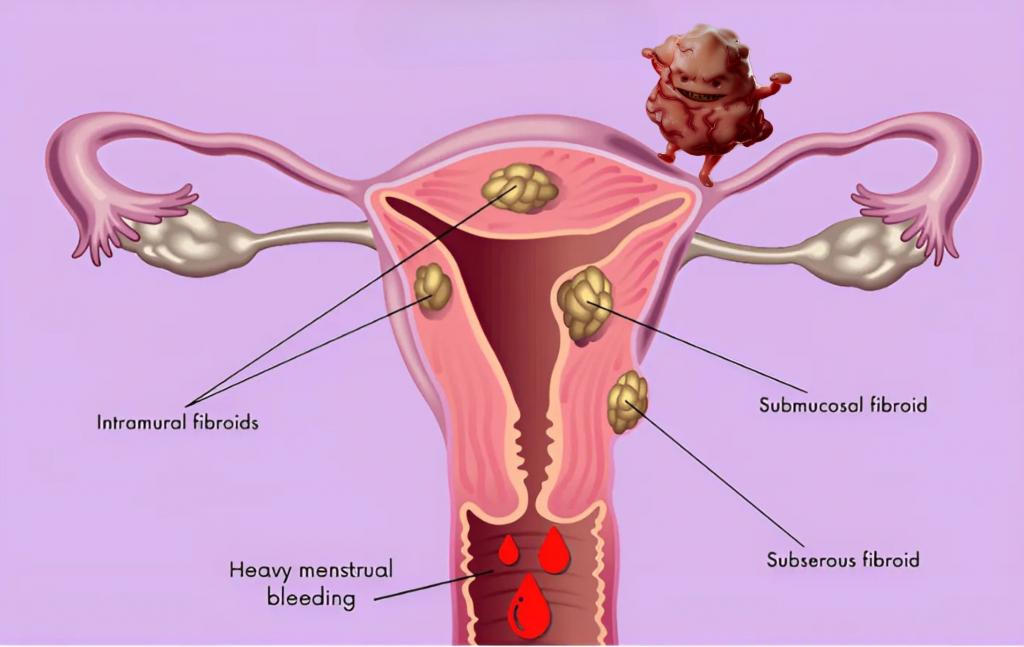
Another major factor is the development of gynecological conditions. Fibroids, for example, are benign growths in the uterus that can cause heavier bleeding, severe cramps, pelvic pressure, and lower back pain. They often develop or enlarge during your reproductive years, peaking in prevalence during your late 30s to early 50s. Endometriosis, where tissue similar to the uterine lining grows outside the uterus, is another leading cause of worsening menstrual pain, as is adenomyosis, a condition where that lining tissue grows into the muscular wall of the uterus. Even pelvic inflammatory disease, often the result of untreated infections, can create lasting pelvic discomfort that intensifies during menstruation.
Lifestyle also plays a role. High stress levels, a sedentary routine, and diets high in inflammatory foods can make cramps feel worse over time. Our bodies’ ability to bounce back from monthly discomfort can decline when overall health and wellness are neglected.
Common Reasons Period Cramps Get Worse With Age
1. Uterine Fibroids
Fibroids are noncancerous growths of the uterus that commonly appear during your reproductive years — especially between ages 30 and 50. They can cause intense cramping, prolonged bleeding, and pressure in the lower abdomen.
2. Adenomyosis
This condition occurs when the uterine lining grows into the uterine wall, thickening it and making each period more painful.
3. Endometriosis
When uterine-like tissue grows outside the uterus, it leads to chronic inflammation, pelvic pain, and cramps that worsen with age.
4. Hormonal Changes in Perimenopause
As estrogen and progesterone levels fluctuate, uterine tissue may thicken or bleed irregularly, leading to heavier periods and stronger cramps.
When Is It Normal and When Should You Be Concerned?
Some increase in discomfort over time can be part of the natural aging process, but a significant shift in your pain pattern is worth paying attention to. If your cramps suddenly become much more intense, occur outside of your menstrual days, or are accompanied by unusually heavy bleeding, large blood clots, or fertility issues, it’s time to speak with a healthcare professional. These symptoms can indicate fibroids, endometriosis, or other treatable conditions — and catching them early often leads to better outcomes.
How Doctors Diagnose the Worsening Period Pain with Age Cause
When worsening period pain becomes disruptive, your doctor will start by reviewing your symptoms and performing a pelvic examination. Imaging tests such as ultrasound are often used to check for fibroids, cysts, or uterine thickening, while MRI scans can give a more detailed look at the uterus and pelvic organs. In some cases, laparoscopy — a minimally invasive surgical procedure — may be recommended to confirm endometriosis. Hormone testing can also help identify imbalances that might be contributing to your symptoms.
How Fibroids Cause Painful Periods and When to Consider UFE
Fibroids are one of the most common causes of worsening menstrual cramps in women over 30. Depending on their size and location, they can put pressure on the uterus, interfere with blood flow, and make uterine contractions more painful.
If your period cramps are linked to fibroids, it’s important to know that relief is possible — and you don’t need surgery to get it.
At USA Fibroid Centers, we offer Uterine Fibroid Embolization (UFE), a non-surgical, outpatient procedure that targets the root cause of fibroid pain.
UFE works by blocking blood flow to fibroids, causing them to shrink and symptoms to fade — without removing the uterus.
What Age Can You Get UFE?
Most women who undergo UFE are between ages 23 and 58, though suitability depends on your overall health and reproductive goals. UFE is ideal for women who:
-
Experience heavy or painful periods due to fibroids
-
Want to preserve their uterus
-
Prefer a non-surgical treatment with a fast recovery
If you’re approaching perimenopause or have completed childbearing, UFE can be an excellent alternative to hysterectomy — providing long-lasting relief without major surgery.
Call to Schedule a Fibroid Consultation
Managing Worsening Period Pain
Addressing this kind of pain often involves a combination of self-care and medical treatment. Heat therapy, such as using a warm compress or heating pad, can relax uterine muscles and improve blood flow. Gentle exercise and stretching can release endorphins, which act as natural painkillers, while an anti-inflammatory diet rich in leafy greens, omega-3 fatty acids, and whole grains may help reduce discomfort over time.
Medical options vary depending on the underlying cause. Non-steroidal anti-inflammatory drugs (NSAIDs) can reduce prostaglandin levels and ease cramps. Hormonal birth control is sometimes prescribed to regulate cycles and reduce bleeding. For fibroids, procedures such as myomectomy (surgical removal) or uterine artery embolization (blocking blood supply to shrink fibroids) can be effective. If adenomyosis or endometriosis is diagnosed, surgical intervention might be necessary to remove the affected tissue.
Preventing Long-Term Complications
The key to preventing period pain from taking over your life is early intervention. Tracking your cycle, noting changes in your pain, and maintaining regular gynecological check-ups can make it easier to spot problems before they escalate. Supporting your body with balanced nutrition, regular movement, and stress-reduction techniques also helps reduce inflammation and keeps your hormones more balanced.
Conclusion
Period pain that worsens with age should never be dismissed as “just part of being a woman.” While hormonal changes can cause some discomfort, conditions like fibroids, endometriosis, and adenomyosis are common causes — and they’re treatable. Listening to your body, seeking timely medical advice, and making healthy lifestyle adjustments can help you regain control of your cycle and improve your overall quality of life.